Customer Experience
- Target the right customers
- With the right message and content
- Through the right channels
- In the right format
- At the right time
- In the right way (Compliant)
Measure your identity data management maturity. Take our 5-minute maturity assessment now
Avoided costs
$585,000 in annual cost savings & $990,000 in upfront cost savings
Increased “Click Rate”
Improve email click rate by 24%
Enhanced productivity
Automatically resolve over 70% of match related tasks
Demographic Data Enhancement
Capture 40% more attributes compared to other 3rd party data vendors
Closing gaps in care
35% improvement in conversion from care gaps campaign

Verato helps organizations throughout the merger & acquisition lifecycle obtain an accurate and complete picture of a patient, consumer, provider & organizational entity.
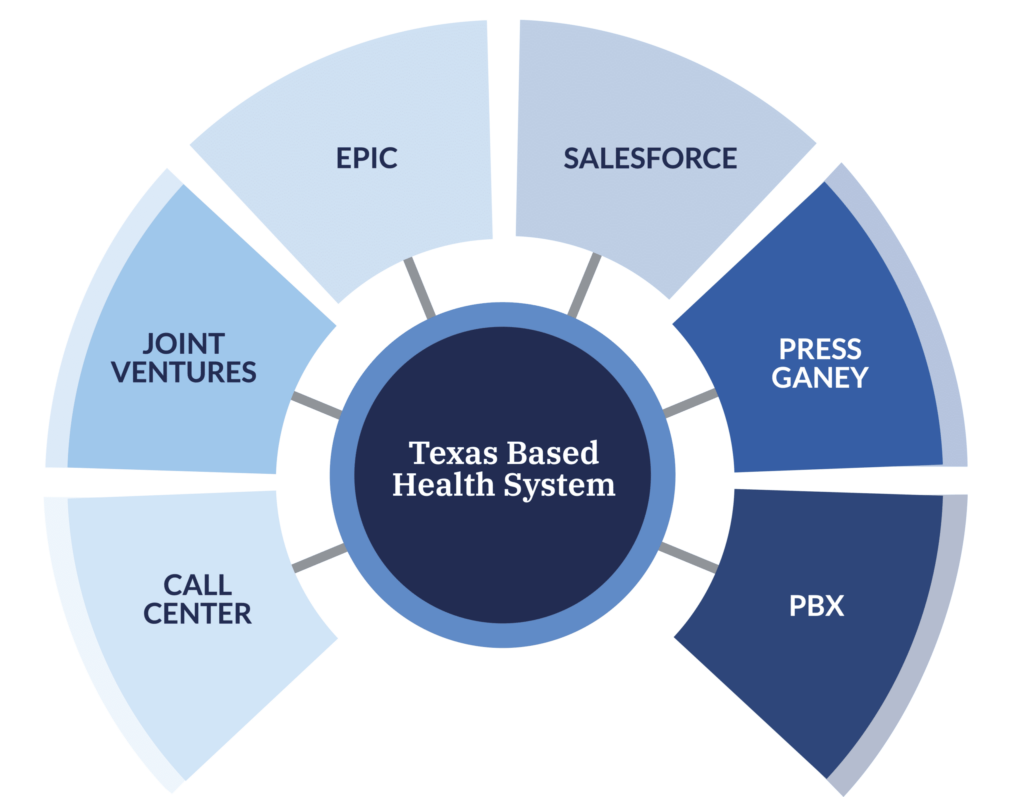
Data enters this organization’s EDW from various feeds and at various frequencies (e.g. Epic runs every morning and every night), and all data is sent to Verato from the health system’s ETL layer prior to being loaded into the EDW — calling this organization’s private instance of the Verato hMDM platform via Verato’s RESTful web-services APIs for real-time assignment of a unique ID called a LinkID.
Verato uses Verato Referential Matching technology in the health system’s private hMDM instance to determine if each record belongs to a new or existing patient before assigning the LinkID in real time This health system uses the LinkID in the EDW as the unique key to join all the data about a person together to power its marketing and analytics initiatives. This organization stays in sync with LinkID assignments automatically and in real time via API.
“Verato allows us to create a unified view of our consumers so we can connect people to the right care at the right time across our systems. We originally looked at Verato as an EMPI for our EDW, but we’re finding it has flexibility far beyond that use case, which allows us to be nimble across our initiatives.”